Imagining the Future of Outpatient Care Environments
Priya Malhotra AIA, LEED AP BD+C
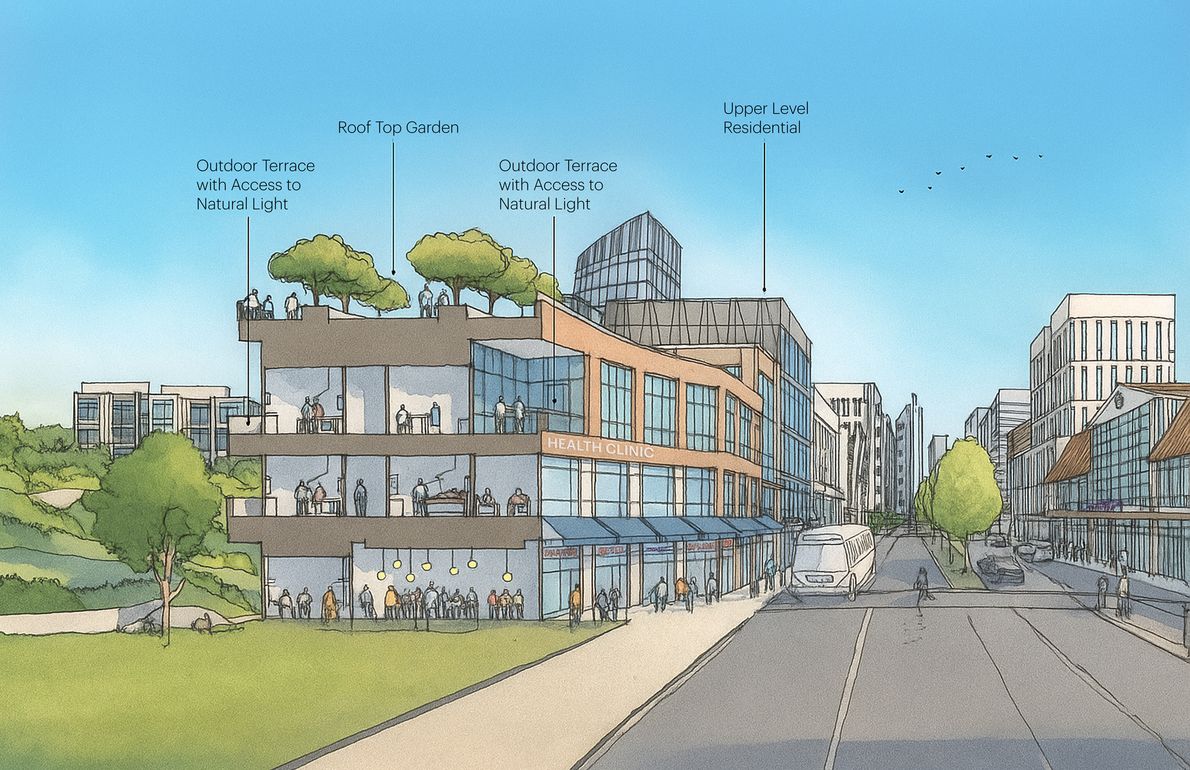
Conceptual Clinic located within an existing mixed-use commercial building in an urban environment, with access to public transportation and other public amenities.
Developed in collaboration with Gloria Breck, DES
As the demand for healthcare services continues to grow while resources remain constrained, the future of outpatient care will depend on our ability to make care environments both deeply human-centered and highly efficient. Designers, operators, and developers must navigate this intersection thoughtfully—balancing human experience with automation and emerging technologies.
Traditionally, Medical Office Buildings (MOBs) served as extensions of hospitals, housing physician practices and diagnostic services. Today, they are rapidly transforming into multi-functional outpatient care environments that support prevention, wellness, and community-based care. These new models are redefining how and where people access healthcare.
According to the U.S. Census Bureau, the number of Americans aged 65 and older is projected to nearly double by 2050, driving growing demand for healthcare services focused on prevention, wellness, and accessibility.
Healthcare delivery is also shifting from inpatient hospitals toward outpatient and community-based facilities. Minimally invasive procedures, payer incentives, and patient expectations for convenience are moving care into Ambulatory Surgery Centers (ASCs), urgent care, and specialty clinics. Between 2023 and 2025, the Centers for Medicare & Medicaid Services added nearly 60 new procedures to the ASC payable list—all clear signals of the ongoing decentralization of care and the need for human-centered outpatient environments.

Sutter’s Blossom Hill Clinic in San Jose makes community healthcare accessible by repurposing a retail lighting store into a family medicine and specialty outpatient facility.
The Next Generation of Outpatient Buildings
If healthcare is moving toward prevention, personalization, and accessibility, tomorrow’s outpatient environments may look very different from the large, centralized medical office buildings we know today.
- Embedded in everyday life
Clinics may increasingly be located within pharmacies, workplaces, schools, or mixed-use developments; places people already frequent, as seen with Crossover Health, Walmart Health, and One Medical. This integration blurs the boundary between healthcare and daily living, bringing preventive care closer to patients and reducing barriers to access. - Integrated health destinations
The traditional boundaries between clinical care, wellness, and community life are dissolving. Future outpatient environments may combine wellness centers, fitness facilities, behavioral health services, imaging, and outpatient surgery within a single location. These multi-service destinations create a seamless continuum of care, connecting prevention, treatment, and recovery, and positioning healthcare as an active part of everyday life. - Supported by intelligent systems
Technology will streamline operations rather than dominate them. Automated check-in, wearable devices that track key health metrics, and data-driven predictive tools will help providers anticipate patient needs, optimize scheduling, and improve overall care.
- Smaller, smarter, and more flexible
Future outpatient facilities will be right-sized and adaptive. Modular planning, shared clinical support zones, and mobile equipment will allow rapid reconfiguration as procedures and technologies evolve. Robotics can support back-of-house operations such as supply delivery or instrument sterilization, freeing up more space for patient care and staff respite. - More humane, more biophilic
Even as care becomes more digital, the need for human connection and natural environments will grow. Expect courtyards, daylight-filled waiting areas, and restorative staff spaces integrated into clinical settings—design elements that promote both healing and well-being. - Equipped for hybrid care
The pandemic accelerated acceptance of telehealth and hybrid care models. Future outpatient environments will incorporate soundproof teleconsultation rooms, secure digital infrastructure, and flexible scheduling systems that support seamless transitions between virtual and in-person visits. - Designed for sustainability and resilience
As healthcare expands into communities, outpatient environments must embody environmental responsibility. Energy-efficient systems, renewable power, low-water landscaping, and adaptive reuse should be core design principles to reduce the carbon footprint. Sustainable design also supports well-being: enhancing air quality, access to daylight, and long-term resilience during climate-related events.
Designing with Intent
The evolution of outpatient care requires collaboration across architecture, healthcare operations, and technology. Rather than measuring success purely by cost per square foot, we must align design values with the broader goals of healthcare itself: accessibility, equity, sustainability, and human dignity.

Priya Malhotra AIA, LEED AP BD+C
Associate | Project Manager









